Groundhog Day and Seasonal Affective Disorder
There are things you can count on, and each year, Groundhog’s Day is one of them. On the morning of February 2, Punxsutawney Phil, an actual groundhog, will emerge from his warren in Punxsutawney, Pennsylvania, to predict a wonderful early spring or a dreaded 6 more weeks of winter. Last year, Phil saw his shadow, and a lengthened winter was ahead of us. Most of us don’t fully believe that Phil is the ultimate source for such a prediction, but even hearing the potential of a longer winter can cause those of us needing sun and warmth to feel blue and out of sorts. In mental health circles, that feeling can be referred to as SAD, Seasonal Affective Disorder.
SAD is real. It is accepted as a defined disorder by the American Psychiatric Association, and it leads to depression and feelings of sadness. It is known that depression can be debilitating, leading to loss of interest in pleasurable activities, feelings of being stuck and unable to be productive, feelings of being hopeless, helpless, or worthless, anxiousness, weight loss or gain, and even thoughts of suicide.
If you already have depression or anxiety–related symptoms, you may have a higher risk of the winter impacting your mood. Some find that light therapy can improve symptoms, and others find that talk therapies and medication are helpful.
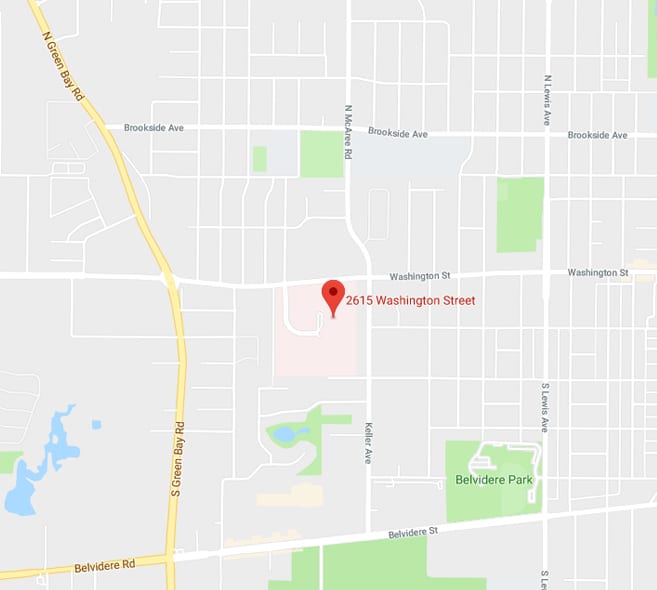
SAD is a diagnosable and controllable condition. Don’t let a groundhog impact your life! If you or a loved one are experiencing depression in any form, please allow the qualified professionals at Lake Behavioral Hospital to help by providing a free, confidential assessment that will help determine the level of care for your symptoms. Call 855-990-1900, 24/7/365, to schedule an assessment. Walk-ins are welcome.